What is urinary incontinence?
Millions of women around the world are suffering from stress urinary incontinence. In France alone, this affects more than 3 million women(1), in the USA the number is estimated to be approximately 24 million(2). Women of all ages are affected: young women, middle-aged women or seniors.
Urinary incontinence can have many different causes, can develop in varying degrees of severity. There are three main types of urinary incontinence, among them we can find also the stress urinary incontinence:
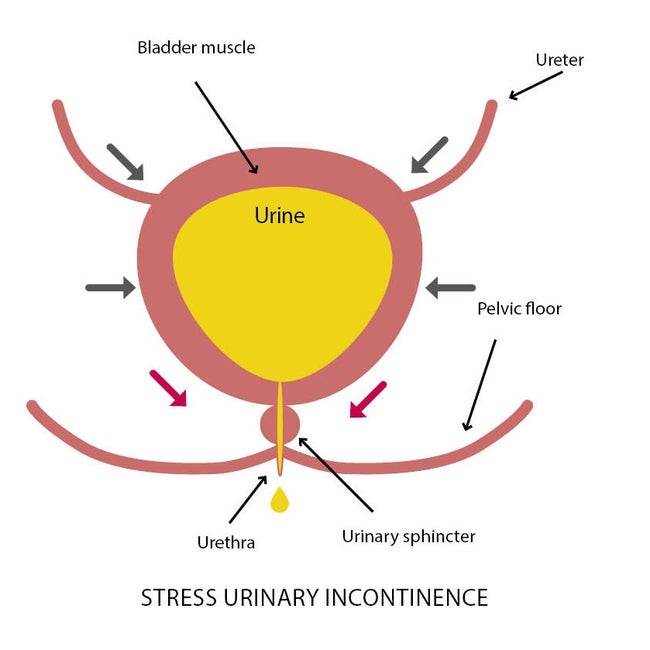
Stress urinary incontinence (SUI)
Stress urinary incontinence (SUI) is the inability to retain urine when laughing, coughing or sneezing.(3,4) SUI occurs when the intraabdominal pressure which suddenly rises and generates a peak of pressure on the bladder.(5) SUI represents 50 to 88 % of all types of urinary incontinence.(6)
Principal causes:
- Current heavy smoking.(7)
- Chronic constipation.(8)
- Giving birth to a heavy child (more than 4 kg) and the number of vaginal deliveries a woman has had may also adversely affect the functional resilience of the pelvic floor.(8)
- Postmenopausal age.(8)
- The use of catheters also increases the risk of damaging the urethral sphincter.(8)
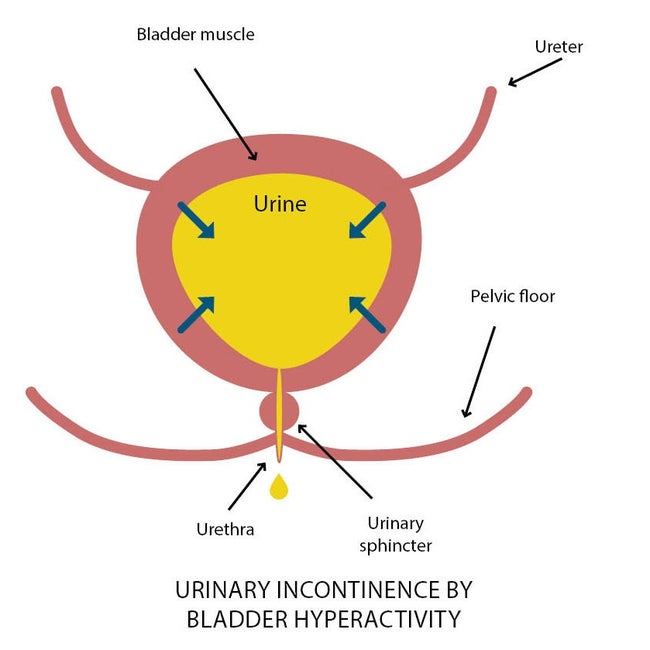
Urinary incontinence by bladder hyperactivity (UUI)
Urge urinary incontinence occurs an involuntary leakage arising for no apparent reason and associated with urgency.(4) It is a strong feeling to urinate even when the bladder isn't full. This can occur in both men and women and involves a strong urge to urinate, often followed by loss of urine before reaching the toilet.
Principal causes:
- Neurological diseases such as Parkinson disease, urinary tract infections or bladder diseases (stones and polyps).
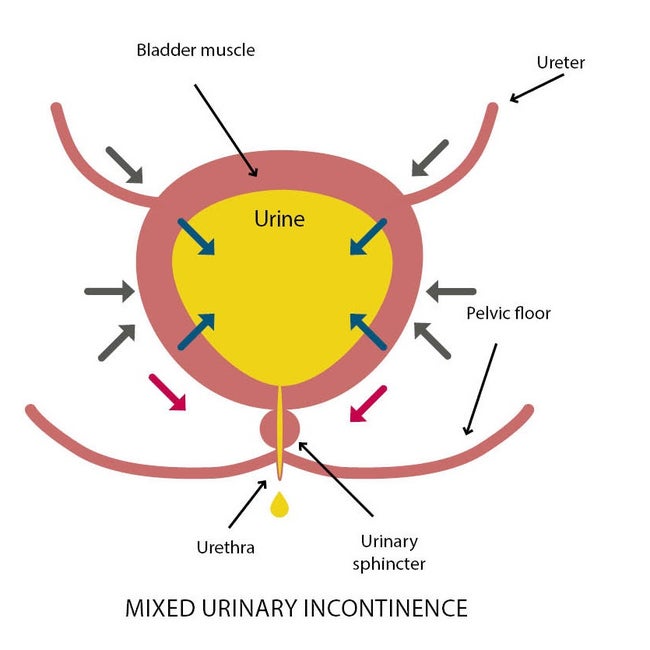
Mixed urinary incontinence (MUI)
MUI is defined as a complaint of the involuntary loss of urine during exertion, sneezing, or coughing, as well as leakage associated with urgency.(4) MUI refers to a combination of symptoms, with the patient exhibiting features of both stress urinary incontinence (SUI) and urge urinary incontinence (UUI).
Principal causes:
- Ageing
- Menopause
- Obesity
- Chronic constipation
- Intensive physical activity
How to deal with stress urinary incontinence?
Nowadays, different well-known solutions such as pelvic floor muscle training and surgery are available to women who suffer from stress urinary incontinence. However, there is no alternative between these two solutions except diapers which are considered as a palliative solution. Despite medical progress on Stress Urinary Incontinence, it is still a taboo topic.
Solutions to deal with stress urinary incontinence:

Pelvic floor muscle training
Pelvic floor muscle training, alone or associated to biofeedback or with electrical stimulation can be done by a physiotherapist or a midwife. It is the first-line treatment indicated to women who suffer from stress urinary incontinence before going to surgery. Pelvic floor muscle training is effective and sometimes heal the patient with small leakages but it is not sufficient for sportive ladies or women who practice intense activities.(9)

Diapers and other protections
Diapers and other protections are available in different sizes and anatomic forms such as absorbent panties and disposable waterproof mattress protectors.(9)
Surgery
Surgery can be recommended by an urologist and/or a gynecologist. It can be proposed in case of absence of improvement of the symptoms after a well-conducted rehabilitation (10 to 20 sessions). Different methods are available: Suburethral strips, bulking agent and artificial sphincters.(9)
And now Diveen®
Diveen®, the innovative non-surgical device that applies like a tampon to apply and reduces incidence of urinary leakages by 69 percent on average.(10)
Related Document
References
(1) https://www.urofrance.org/congres-et-formations/formation-initiale/referentiel-du-college/incontinence-urinaire.html (16.04.2020)
(2) Wu JM, Hundley AF, Fulton RG. Forecasting the prevalence of pelvic floor disorders in US women 2010–2050. Obst Gynecol. 2009;114(6):1278–83
(3) Qaseem A, Dallas P, Forciea MA, Starkey M, Denberg TD, Shekelle P. Nonsurgical management of urinary incontinence in women: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2014;161(6):429–40. doi:10.7326/M13-2410.
(4) Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology. 2003;61(1):37–49. doi:10.1016/S0090-4295(02)02243-4.
(5) Wang A, Carr LK. Female stress urinary incontinence. Can J Urol. 2008;15 Suppl 1:37-43; discussion 43.
(6) Kołodyńska G, Zalewski M, Rożek-Piechura K. Urinary incontinence in postmenopausal women - causes, symptoms, treatment. Prz Menopauzalny. 2019;18(1):46–50. doi:10.5114/pm.2019.84157.
(7) Hannestad YS, Rortveit G, Daltveit AK, Hunskaar S. Are smoking and other lifestyle factors associated with female urinary incontinence? The Norwegian EPINCONT Study. International journal of Obstetrics and gyneacolgy. 2003;110:247–54.
(8) Bernards ATM, Berghmans BCM, Slieker-Ten Hove MCP, Staal JB, Bie RA de, Hendriks EJM. Dutch guidelines for physiotherapy in patients with stress urinary incontinence: an update. Int Urogynecol J. 2014;25(2):171–9. doi:10.1007/s00192-013-2219-3.
(9) Rapport sur le thème de l'incontinence urinaire - Pr. F. Haab 2007
(10) Cornu J.N et al. 75NC007 device for noninvasive stress urinary incontinence management in women: a randomized control trial. International Urogynecology Journal 2012.