Short Stitch - A small stitch with a big impact
For decades, the relevance of fascial and wound closure received only cursory scientific study.
However, abdominal wall rupture rates of up to four percent, a wound infection rate of up to 25 percent and an incisional hernia frequency after one year of up to 36 percent following elective abdominal surgery as reported in the literature demands for improvement.
The previous gold standard in abdominal wall closure was a continuous 4:1 suture length/ wound length ratio (SL/WL ratio), usually with a deep (full-thickness), monofilament 0/1 loop suture. Now, a prospective, randomized, multicenter trial (STITCH) published in 2015 has found that opting for a > 4:1 short stitch technique for an elective, midline abdominal wall closure reduces the incisional hernia rate from 21 to 13 percent 1. The implementation of this procedure would lead to a break with virtually all previous traditions in elective abdominal wall closure—at least at the midline. The 0/1 loop is replaced with the 2-0 suture, which is around 50 percent lighter, and the stitch technique is changed from a deep, combined musculo-fascial suture to an isolated fascial suture in the linea alba. This is accompanied by a switch from the large 33/45 needles to smaller 26/30 needles in order to better estimate lateral suture distance, depth and interval.
The recommendation for the short stitch technique by the European Hernia Society (EHS) in 2015 was made based on moderate evidence from experimental studies on animal models and a prospective clinical trial, and has now been supplemented by a high-quality, prospective, randomized analysis (STITCH study) 1, 2. The study data now recommends a > 4:1 short stitch technique.
More surprising than the result is the fact that four decades had to pass before enough data was generated to convince an increased number of surgeons to accept these technical modifications as a rule, although there is substantial doubt that they will comply and change old habits of closure technique. Nevertheless, the data clearly show that surgeons should part with the highly familiar, easily performed, and firmly pulled suture with large needle and loop. The small needle and significantly thinner suture are compatible with regard to tear-out force, sensible in terms of practicality and encourage the short stitch technique to be performed in a technically adequate manner.
That this also means a negligible extension in operating time by 10 minutes on average needs to be accepted is cost-efficient, with regard to both direct and indirect costs 3.
„Short Stitch 6:1-Monomax“-trial
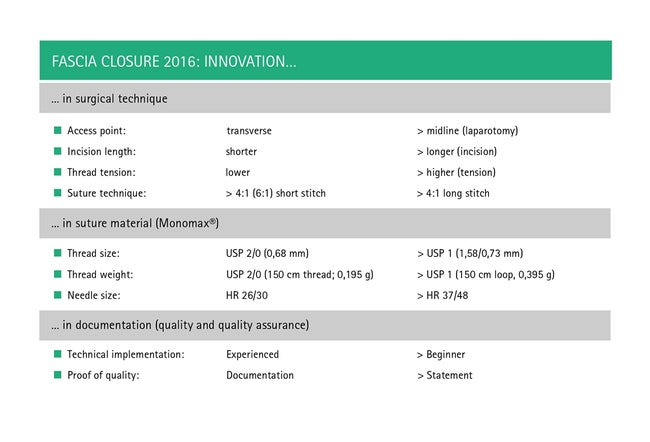
With regard to the anticipated positive results of the STITCH trial, a prospective, monocentric trial of monofilament suture material for fascial closure (poly-4-hydroxybutyrate, Monomax, B. Braun) commenced back in 2012. In addition to further increasing the SL/WL ratio (6:1), this trial was the first to investigate expanding the indication to include transverse, emergency and relaparotomies. Technically, the difference first appeared marginal. The somewhat more laborious 6:1 technique, however, can make the suture appear like a zipper under certain circumstances. The obligatory counting of the sutures while applying the technique remained essential, since otherwise long stitch and short stitch techniques cannot be adequately distinguished (Table 1).
The evidence for the short stitch technique has so far only pertained to midline laparotomies. For the Short Stitch 6:1 Monomax trial, the technical difficulty is in properly performing the technique during relaparotomies and, above all, for transverse laparotomy closure. For the former, the incision and for the latter, the two-layer implementation with dorsal fascial weakness, the unavoidable biting of muscle tissue at the fascial fusion between dorsal and ventral fascia on the linea semilunaris has to be taken into account (Table 2). Experience has shown that the short stitch technique has also been proven for a separate suture of the ventral and dorsal layers, however the 6:1 ratio is even more difficult to achieve than in the midline suture.
The 2-0 suture with the HR 26/30 needle also lends itself to the 6:1 short stitch technique. This reduces suture weight and thread size with comparable tear-out force. The authors of this article prefer the HR30 needle, since the often incorrectly estimated lateral stitch edge should be between five and eight millimeters, and this corresponds to around half the diameter (Table 3).
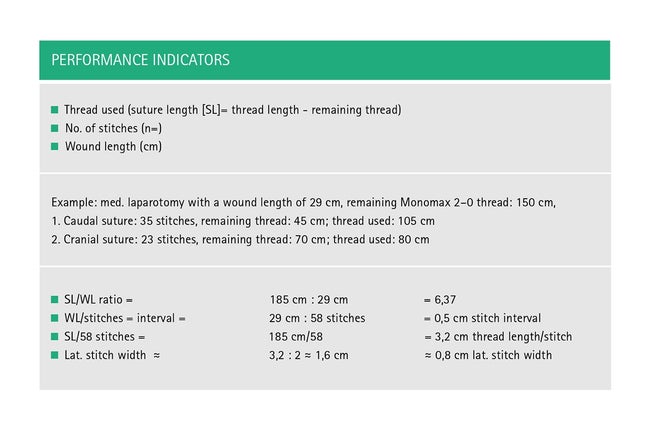
Another factor is the tension. In the experiment on animal models, increased tension on the thread reduced early and late tear-out force (wound thickness). Internal clinical studies with a tensiometer showed that the retaining force on the thread can be up to 50 N. Based on the very high tear-out force of > 100 N, this is not a problem with poly-4-hydroxybutyrate thread (Monomax). However, tension over 20 N is technically relevant since the associated loss in the suture material's generally longitudinal elasticity through elongation (elongation = loss of elastic recoil) becomes evident. In our first clinical trials, the approximation of the fascia could be sufficiently reached without difficulty at tensions well below 5 N. This is also the most effective prophylaxis for avoiding what are called "button holes". Over the past three years, the authors of this article have consistently employed the short stitch technique in elective and emergency surgeries and the results have been positive throughout. Abdominal wall rupture has become a rarity (0.5 percent), anastomotic leaks have no visible effect on secondary wound dehiscence. However, the additional work at the end of the operation requires educational measures for fellow doctors and nurses. This concerns the preparation of an eight to ten millimeter section of the bilateral epifascial space with clear identification of fascial, muscle and adipose tissue boundaries, the separation of the incision as a potential weak point in the fascia and, of course, the diligent documentation of the performance indicators (Table 1).
Implementing the short stitch technique
What is decisive for the implementation of the short stitch technique in its standardized application is less the shift in evidence and the proclaimed change in guidelines, rather whether it can be effectively implemented overall. But there's one more hurdle: As studies have shown, the sole argument for using this technique is not enough. This is because the scientific principle of documenting methodical approaches and results holds true, i.e., recording the stitches, the sutures used (SL) and the wound lengths (WL). This helps the surgeon check their own success (learning curve) and ensure quality (tables 1 and 3). While doing so, the initial and final knots suggested by Israelsson are recommended, as they make it easier to measure the leftover suture lengths. The trial conducted by Israelsson et al.4 also showed that there's a substantial difference in interpersonal and intrapersonal quality, and deficiencies can be improved by documentation (plan–do–check–act [PDCA] learning).
Summary
- The > 4:1 short stitch technique has the potential of becoming the gold standard for midline laparotomies.
- The 6:1 short stitch technique is an advancement.
- Even transverse and emergency relaparotomies can be successfully taken care of.
- Reducing tension to < 5 N is recommended (elastic recoil, "button holes")
- Monomax 2-0 is an indicator suture for correct tension (technique quality).
- Quality assurance (documentation) reduces the learning curve (PDCA).
- The goal of future suture trials will be to precisely determine the target size and to standardize all other factors (e.g., suture material, suture technique, access).
Outlook
Pending a general recommendation for the short stitch technique for all fascial closures (transverse laparotomy, Pfannenstiel incision, relaparotomy and emergency laparotomy), there's still a lack of appropriately broad evidence. Previous relevant trial results pertain only to a midline, elective, primary laparotomy. At present, the short stitch technique is under evaluation with Monomax in > 4:1 (ESTOIH trial) and 6:1 (Short Stitch 6:1 Monomax trial) at multiple and individual sites for elective, midline and, generally, all types of access and levels of urgency.
Conclusion for practice
"Less is more": Less material (isolates the fascia), smaller incisions, less tension on the suture and less tension between fascia and suture
"More is also more": Higher SL/WL ratio, more documentation (quality assurance), more filing and well-structured trials
By Dr. Markus Golling, Sebastian Felbinger and Zofia Zielska
References
1. Deerenberg EB, Harlaar JJ, Steyerberg EW, Lont HE, van Doorn HC, Heisterkamp J, Wijnhoven BP, Schouten WR, Cense HA, Stockmann HB, Berends FJ, Dijkhuizen FP, Dwarkasing RS, Jairam AP, van Ramshorst GH, Kleinrensink GJ, Jeekel J, Lange JF. Small bites versus large bites for closure of abdominal midline incisions (STITCH): a double-blind, multicenter, randomized controlled trial. Lancet. 2015 Sep 26; 386 (10000): 1254–60.
2. Muysoms FE, Antoniou SA, Bury K, Campanelli G, Conze J, Cuccurullo D, de Beaux AC, Deerenberg EB, East B, Fortelny RH, Gillion JF, Henriksen NA, Israelsson L, Jairam A, Jänes A, Jeekel J, López-Cano M, Miserez M, Morales-Conde S, Sanders DL, Simons MP, Smietanski M, Venclauskas L, Berrevoet F; European Hernia Society. European Hernia Society guidelines on the closure of abdominal wall incisions. Hernia. 2015 Feb;19(1):1–24.
3. Millbourn D, Wimo A, Israelsson LA. Cost analysis of the use of small stitches when closing midline abdominal incisions. Hernia. 2014;18(6):775–80.
4. Israelsson LA, Millbourn D. Closing midline abdominal incisions. Langenbecks Arch Surg. 2012 Dec; 397 (8): 1201-7.














