The crisis as catalyst
The coronavirus pandemic took the world by surprise - and would bring daunting tasks for health care systems to face. The value of new processes needed to be proven, resources were temporarily scarce.
In this situation, it quickly became clear that health care providers, the health care industry, scientists and medical practitioners would have to double their efforts while remaining flexible so they could meet the challenges that would continually present themselves. More than a year after the start of the pandemic, the virus is still not under control—though there has been a silver lining in that the crisis has brought about changes from which everyone will benefit. Here are three propositions on how the pandemic is acting as a catalyst.
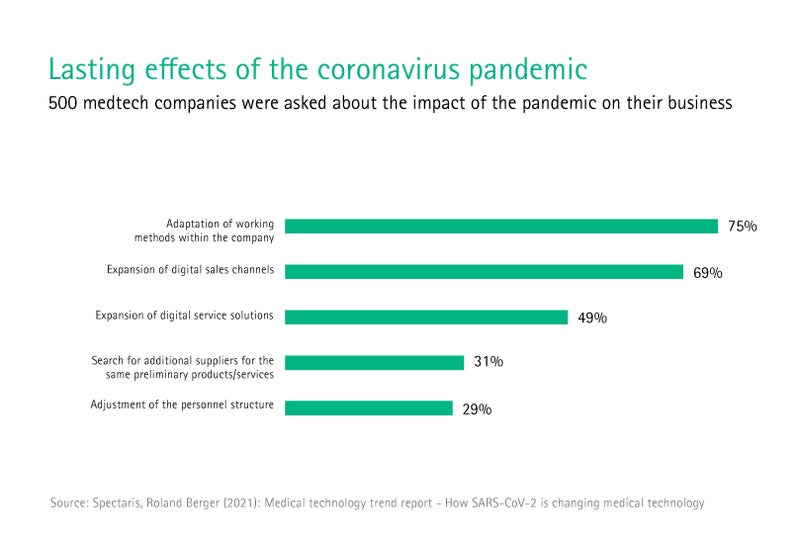
1. The digitalization of health care is accelerating and the public’s openness to digital technologies is growing.
Back in the first days of the pandemic, it was obvious that two things would be decisive in the fight against COVID-19: reducing social contact; and being able to react quickly to new developments. In this regard, digital tools and processes in health care are of vital importance.
In Asia, investment in medical technology doubled in 2020 compared to the previous year, in digitally driven startups above all. In China, one example is the success of the platform WeDoctor, which provides remote consultation hours. Compared to the previous year, the number of digital consultations on this platform rose by a factor of 3.6. In South Korea, 22,000 of the 23,000 pharmacies in the country reported their inventories of FFP2 masks to a government app that was swiftly developed right at the start of the pandemic, allowing the pharmacies to avoid lines forming outside.
Digital solutions also help communicate infection rates in real time. The Surveillance Outbreak Response Management and Analysis System (SORMAS) is a long-standing system for reporting and tracking infectious diseases. It was developed by epidemiologists at Germany’s Helmholtz Center in 2014 to contain the Ebola epidemic in West Africa. It is also being used in countries such as Switzerland and France—and increasingly in Germany—to fight the novel coronavirus.
Digitalization is playing an increasingly important role in German health care as well. Since April 2020, hospitals have been reporting their daily bed capacity to a central register, making it possible to detect regional shortages early and avoid them. The National Association of Statutory Health Insurance Physicians reports that, in the first months of the pandemic, around 25,000 medical practices were offering online consultation hours—up from just 1,700. German public health departments are slated to receive € 4 billion in funding by 2026, of which € 800 million is earmarked for digitalization.
Anna Maria Braun, the CEO of B. Braun, sees the pandemic as a watershed: “We're seeing how the public is extremely open to digital technologies and how much these technologies can help us make our processes more efficient and simpler. We need to take advantage of this openness - while still preserving core aspects such as data protection - in order to establish key digital technologies in Europe that are already competitive elsewhere in the world.”
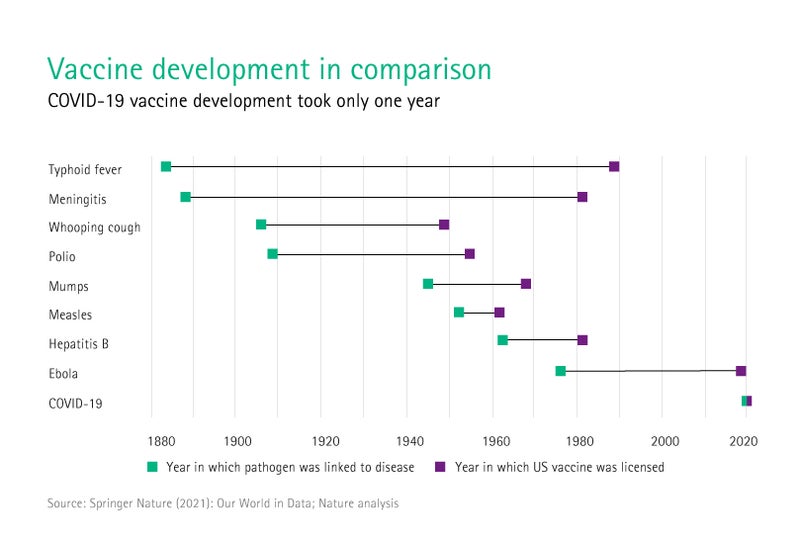
2. Data-driven research and approval processes are increasing the rate of innovation and require international cooperation.
In early January 2020, Chinese researchers published the genome for the SARS-CoV-2 virus—and the global search for a vaccine began. On December 2, the first vaccine for COVID-19 was approved, and others followed in the subsequent weeks and months.
This success, however, was only the most visible result of a much larger phenomenon: The international research community has never worked together as closely and as quickly as it is doing today. Around the world, scientific journals are publishing the latest findings from coronavirus studies at no charge and as quickly as possible. More than 30,000 preprints on COVID-19 were published in 2020. Even the peer-review process for these publications took only half as long for these articles than for other topics; it took a total of just 72 days. These data-driven processes are speeding up the rate of innovation, and other fields of research can benefit from these experiences and infrastructures.
The pandemic has strengthened international cooperation, not only when it comes to research, but also when it comes to health policy. Voluntary increases in contributions have put $ 8.48 billion at the WHO’s disposal for 2020/21—almost double the amount for 2018/19. Another example of real-life solidarity comes from the EU, where ICU patients were being and continue to be moved to Member States with sufficient capacity to receive treatment. The international vaccine initiative COVAX has also received € 6.3 billion in funding so far to provide vaccines to the 92 poorest countries in the world. Since the start of March 2021, a total of 12 million doses have already been distributed. Even though policy decisions regarding health are often made at the national level, a global mindset and action on a global scale are more important than ever.
3. Through the pandemic, governments and societies are finding a new appreciation for their health care systems and are ready to invest in long-term solutions.
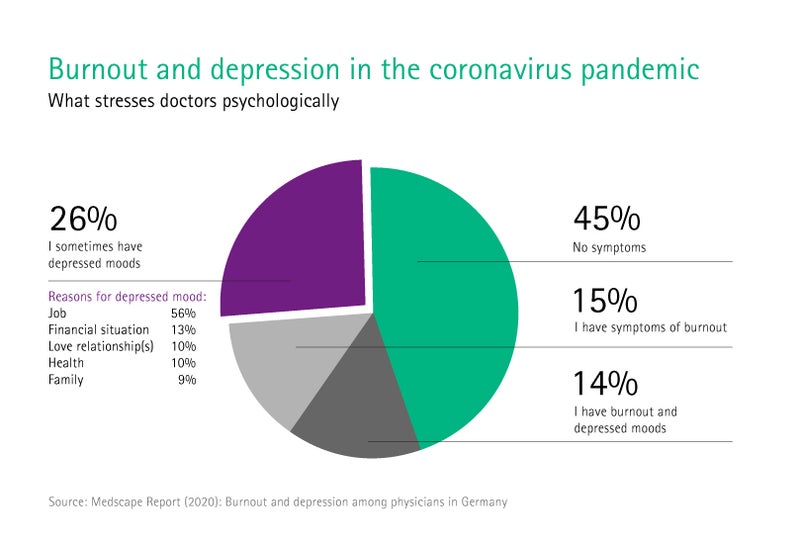
Health care workers do the extraordinary—and not just since the outbreak of the coronavirus. Pictures of utterly exhausted doctors and nurses in the areas hit hardest by the pandemic—Wuhan, Northern Italy, London and New York—that spread around the world in the spring of 2020 changed how the profession is viewed. Health care workers were celebrated in the press and by the public, and rightly so.
The heroism, however, also has a dark side: Those working in COVID-19 wards are more likely to experience depressive symptoms and post-traumatic stress symptoms than their colleagues in normal wards, according to a study by Italian researchers published in the “Journal of Evaluation in Clinical Practice”. The pandemic, therefore, has led to a known problem gaining new relevance: hospital working conditions.
After the pandemic, a return to the status quo is almost inconceivable. The people who care for the public’s health must not be allowed to jeopardize their own in the process. This is why we must come up with sustainable approaches to making health care more efficient and resilient: with adequate human and material resources, flexible working time models, new technology and safety solutions.
The time is ripe for appropriate reforms and investments: People all over the world are more satisfied with their national health care systems one year after the start of the pandemic than they have been in a long time. According to the “Global Health Service Monitor 2020”, around 9 percent more people than in 2018 agreed with the statement that their health care system guaranteed the best possible treatment. This positive sentiment correlates with a major economic trend of governments worldwide spending more on health care, with spending expected to increase 5 percent each year through to 2023.
In spring 2021, the end of the pandemic appears to be in sight for the first time. And even if the danger of viral mutations or other novel pathogens cannot be completely warded off, we can still take proactive steps to make our health care systems even more ready for global threats.